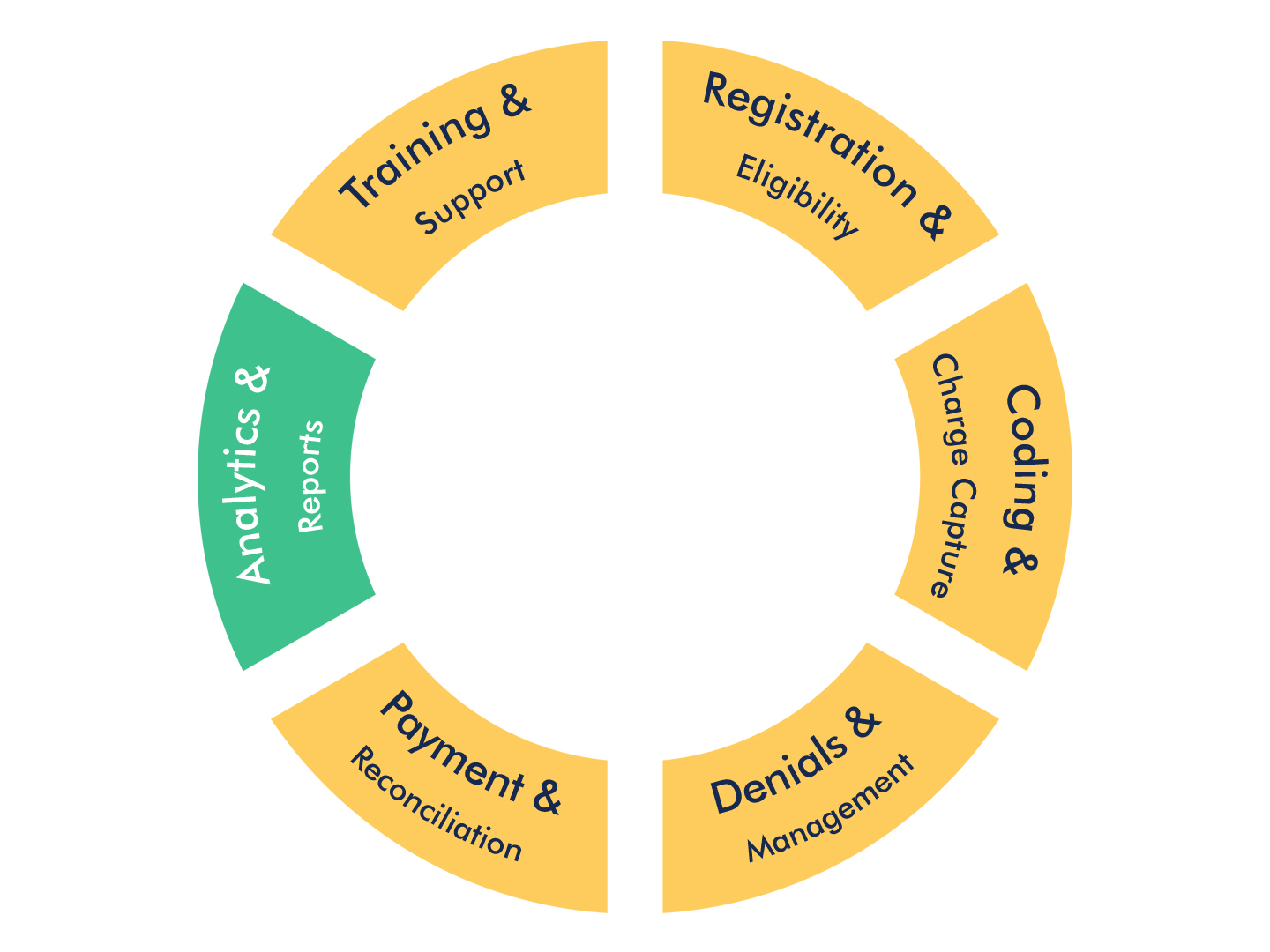
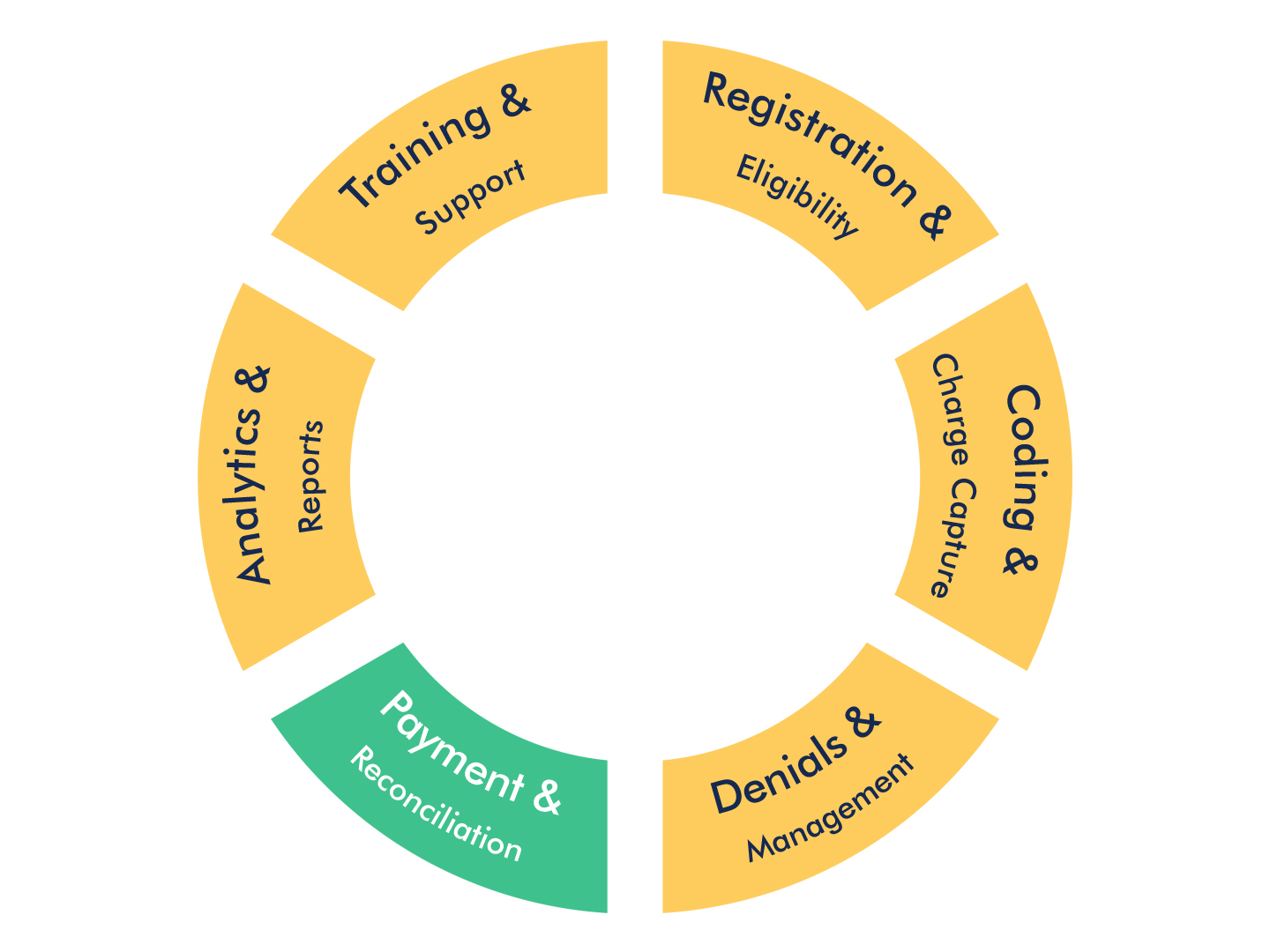
Analytics & Reports
An analytics-driven claims management process provides for fact-based decisions. Once trends are identified they can lead to improvements in the revenue cycle.
Hiccups along the way can delay or prevent payment on claims. The cause can come from patient registration to insufficient documentation and coding errors to payer behavior. Once the origin is identified, analysis can determine were the greatest impact for change lies. Whether it’s a payer, a certain type of code, or a process in need of redesign, the data behind the analysis can help drive decisions that improve the process for faster, higher returns.
The Analytics & Reports services available through the Acentus provide:
- Customizable reports to help diagnose the health of the practice by measuring a variety of KPIs
- Identify trends to determine necessary changes in processes
- Insight into payer reimbursement issues and trends